Code Gridlock: Hospitals “bursting at the seams” heading into flu season
Posted: October 30, 2017
(October 28, 2017)
By: Joanna Frketich, Hamilton Spectator

Hamilton’s hospitals are alarmingly overcrowded before the sickest season of the year even starts.
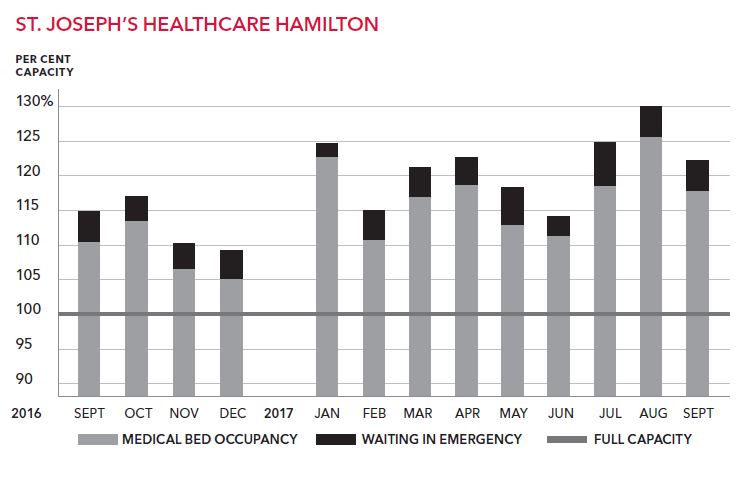
St. Joseph’s Healthcare had 26 per cent more patients than medical beds in August, which is supposed to be one of the quieter months.
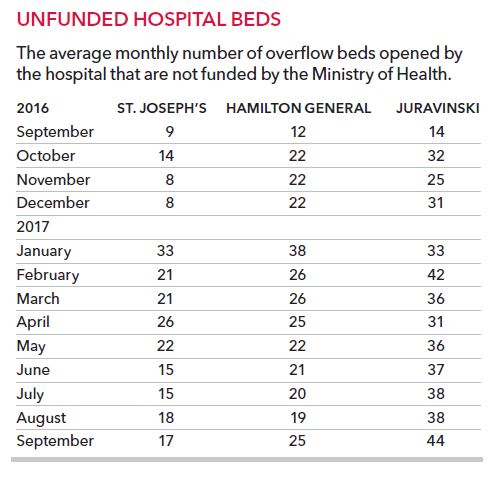
Across the city, hospitals opened an average of 86 overflow beds — some in sunrooms and hallways — in September. These beds are not funded by the province and do not include patients crammed into the emergency department.
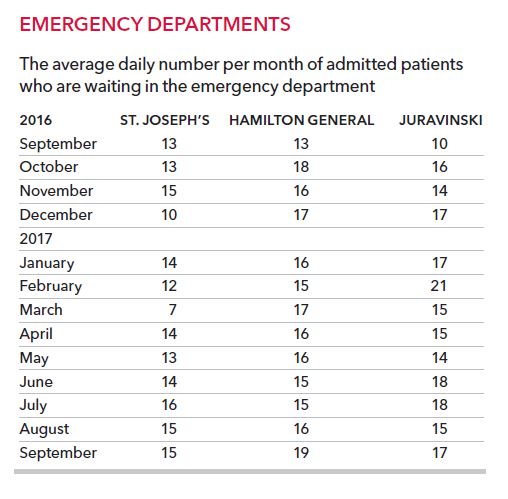
September mornings started off with 51 patients on average stuck in Hamilton’s adult emergency departments waiting for a bed to open on a ward. It means emergency room overcrowding was worse last month than the last flu season.
“They are pretty much bursting at the seams,” said health policy and research consultant Steven Lewis, about Ontario’s urban hospitals. “A system that can’t accommodate a surge in need is a system that is going to get itself in trouble quickly. Every system needs a bit of slack.”
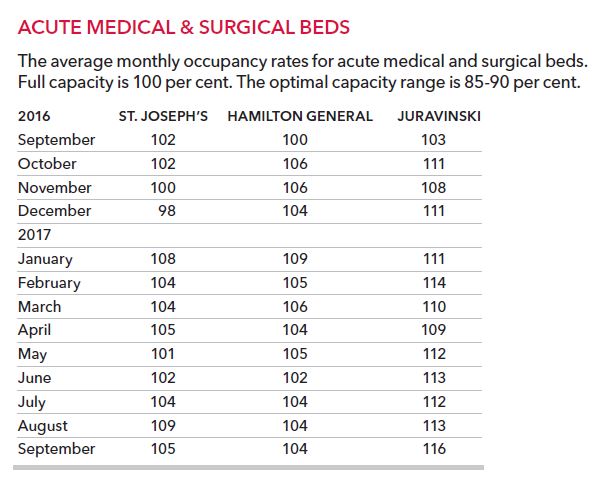
Ideally, hospitals should have an occupancy rate of 85 per cent to 90 per cent, says Lewis, adjunct professor of health policy at Simon Fraser University.
Hamilton Health Sciences has not been below 100 per cent occupancy for 14 months on its adult surgical and medical wards. Juravinski Hospital has been hardest hit, running close to 110 per cent occupancy or higher for a year now.
“The surge never went away,” said Dr. Wes Stephen about the traditionally busy winter season from December to March, which generally slows down in spring and summer.
“This is not unique to Hamilton or Hamilton Health Sciences,” said Stephen, executive vice-president of clinical operations at HHS. “It’s a provincial issue.”
Joseph Brant Hospital did not provide occupancy data to The Spectator, so the situation in Burlington is unknown.
But provincewide, overcrowding has raised questions about what will happen when a flu season predicted to be bad hits hospitals already short of beds.
The Ontario Hospital Association called for “rapid and aggressive new investment” in hospital services in September “to avoid a possible capacity crisis within Ontario’s health-care system this winter.”
It called the prolonged overcrowding “very unusual and worrying” and warned waits for a hospital bed this summer for patients admitted through the emergency department hit the highest monthly level recorded since the province started measuring nine years ago.
“The numbers are obviously of tremendous concern,” OHA president and CEO Anthony Dale told The Spectator. “We do risk toppling over into a crisis this winter with the flu season.”
“Our hospitals are facing increasing demands as a result of our growing and aging population,” said a statement to The Spectator from Health Minister Eric Hoskins’ office. “We’ll need to continue to work closely with our partners at Ontario’s hospitals to determine how we can continue to support them.”
Of those beds, 24 are going to St. Joseph’s Hospital, 15 to Juravinski Hospital, 15 to Hamilton General Hospital and three to the neonatal intensive care unit at McMaster Children’s Hospital, which has also experienced overcrowding in recent months.
While it’s better than nothing, the general consensus is that the beds won’t be enough to meet the coming surge.
“They aren’t even enough to offset the number of unfunded beds being run now,” said Natalie Mehra, executive director of the Ontario Health Coalition. “We don’t believe the beds will be sufficient to meet the needs during the winter and they probably won’t even get hospitals down to 100 per cent (occupancy).”
The added beds won’t fully relieve the gridlock at Hamilton’s hospitals. The funding is for 54 temporary adult beds at a time when 86 extra beds are operating in the city.
“It barely scratches the surface,” said NDP leader and Hamilton Centre MPP Andrea Horwath. “We’ll take the beds and I’m glad they’re finally waking up, but holy smokes, we’ve been ringing the alarm bells for years on this issue. … It can’t continue.”
A big worry is what happens at the end of the fiscal year when the $100 million for the beds runs out. Hamilton’s hospitals have not had one month in the past year when they didn’t have unfunded overflow beds open.
In fact, HHS just hit a high of 121 extra beds — the size of a medium hospital — operating on Oct. 10. It beat out last year’s high of 113.
“The change has been that we have consistently had unfunded beds open now for a very long period of time, so the impact has been cumulative and more significant,” said Winnie Doyle, executive vice-president of clinical services at St. Joseph’s. “There is pressure that comes with all of those extra beds open that is felt across all the services.”
St. Joseph’s had to cancel 16 non-urgent surgeries in the past month because it had no beds. HHS postponed nine surgeries from Oct. 1 to Oct. 10.
A hiring blitz is on at St. Joseph’s because it’s struggling to continually staff the extra beds.
The city is spending $369,842 to temporarily put more paramedics on the road to combat ambulance shortages because paramedics spend too long off-loading patients at congested emergency departments.
“My heart goes out to the families dealing with some of the horrifying situations, whether it’s your 85-year-old mother in a shower room overnight, or your 25-year-old daughter not able to get a bed and sitting in a hallway for five nights,” Horwath said. “Ontarians shouldn’t be getting that kind of health care. It’s an absolute disgrace.”
Lewis agrees hallway medicine is “suboptimal care” and says it will take a lot more than extra hospital beds to fix it.
“The hospitals are the site of the problem, but not the cause of the problem.”
One of the biggest issues is that the long-promised expansion of other types of care — from home care to long-term care to transition care — have not kept pace with shrinking hospital resources.
“The hospital sector has absorbed hundreds of millions in extra costs over the past decade with very little in the way of new funding increases,” Dale said. “We’ve seen some modest increases in the home and community care sector, but not the kind of revolution that is needed.”
As a result, patients ready to be discharged can’t leave the hospital because the kind of care they need isn’t available.
One in five — and at times one in four — of the 287 medical and surgical beds at St. Joseph’s are taken up by patients waiting for other services known as alternate level of care (ALC).
At HHS, it’s closer to one in six of the 549 adult medical and surgical beds at Hamilton General and Juravinski.
Across all the HHS sites, the average number of ALC patients has not been below 150 since the fall of 2015. In recent weeks, it has been as high as 180 to 210 patients.
“This situation has awakened people to the fact that we do need to wrap our heads around the amount of reliance we can realistically place on hospitals over the long term,” Dale said. “It’s definitely affecting staff, especially in areas like emergency where the needs of patients are so intense and there are so many patients that it’s not sustainable for any protracted period of time. Patients are accessing care, but it’s under really stressed circumstances.”
The province is easing some of the pressure with plans to open 860 beds in the community with the aim of getting patients who don’t need to be in hospital discharged. The Oct. 23 announcement included $40 million for post-hospital and preventive care at home.
For Hamilton, it means eight short-term transitional care beds to be run by Wesley Urban Ministries and six by AbleLiving Services. Six Nations Health Services will partner on three supportive housing units.
The biggest investment is nearly $500,000 for 40 affordable housing units at First Place Hamilton, for seniors needing additional community supports when discharged from hospital. The partnership with St. Joseph’s Home Care will provide seniors with rent as well as home and community care supports including assisted living.
Like the temporary hospital beds, it’s an improvement, but a far cry from solving the ALC crisis.
“We need to become extremely serious in Ontario very quickly about building the kind of capacity in the home and community sector, long-term care and building new models of care,” Dale said. “Time is of the essence here.”
jfrketich@thespec.com
Click here for original article