BRIEFING NOTE: The Horrifying Truth About For-Profit Long-Term Care Homes
Posted: December 1, 2021
(December 1, 2021)
Impacts of the COVID-19 Pandemic
As of November 29, 2021, 4,023 residents died as a result of COVID-19 alone. Others died of malnutrition, dehydration, and neglect due to lack of care as COVID-19 rampaged through their long-term care (LTC) homes. Many of the COVID-19 related deaths in LTC homes are also associated with:
- Staff shortages
- Older designs of LTC homes that do not meet modern design standards
- Lack of PPE and infection control
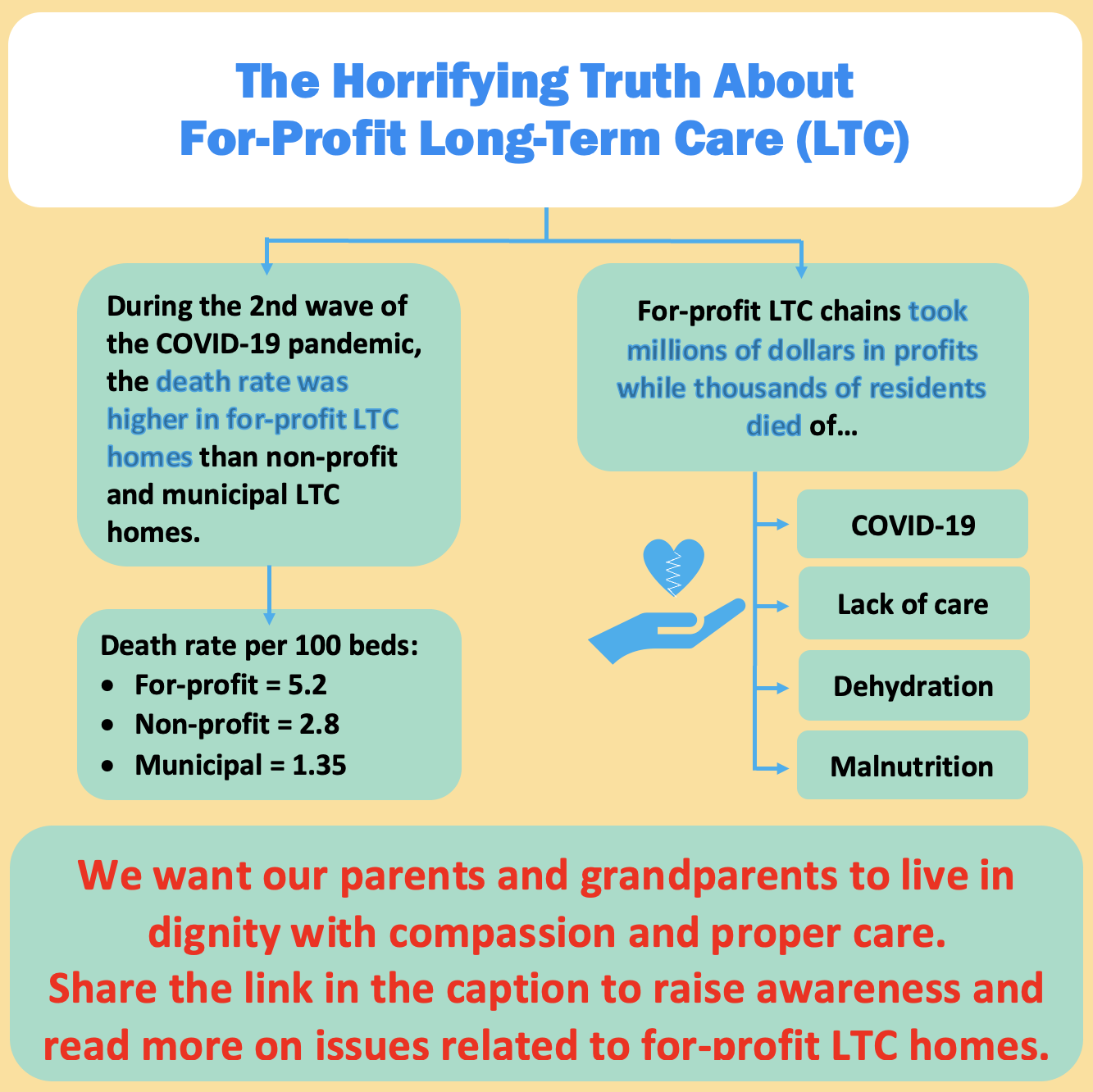
Tragically, many residents died alone. The extraordinary and horrific death rates in for-profit LTC homes expose inadequacies of care and the differences between public and non-profit ownership and for-profit ownership. Some homes did far better though. The fact is that death rates for residents were much higher in for-profit long-term care (LTC) homes than non-profit and publicly-owned LTC homes.
| LTC homes | Death rate per 100 beds
(1st wave and 2nd wave to December 2020) |
| For-profit | 5.2 |
| Non-profit | 2.8 |
| Municipal (Publicly-owned) | 1.35 |
The for-profit LTC homes in Ontario with the highest death rates are owned by Southbridge, Rykka, Sienna, and Revera. These specific corporations have a COVID-19 death rate that is higher even than the average death rate of for-profit LTC homes.
| For-profit LTC chains | Death rate per 100 beds |
| Southbridge | 9.00 |
| Rykka Care Centres | 8.60 |
| Sienna | 6.54 |
| Revera | 6.26 |
Quality of Care
The elderly deserve better. Many residents require care that takes time, but currently, each resident only receives about 2.7 hours of care daily, far less than a safe level of care which would be at minimum 4-hours per resident per day.
The poor quality of care in LTC homes is worse in for-profit LTC homes.
- One study comparing the quality of care between for-profit and non-profit LTC homes found that the hours of direct care residents received in for-profit ownership was 0.34 hours less than the hours of care in non-profit ownership.
- For-profit homes have more cases of diseases and ulcers, complaints, and transfers to hospitals. Residents in for-profit LTC homes are 25% more likely to be hospitalized and 10% more likely to die.
- After a resident spends three months in a for-profit LTC home, their risk of being transferred to a hospital and dying compared to non-profit LTC homes increases to 36% and 20%, respectively.
- A study examined how ownership affects the care outcomes in LTC homes and found that residents in for-profit homes were more likely to be hospitalized with pneumonia, anemia, and dehydration than non-profit LTC homes.
Ultimately, research has shown that ownership is a significant factor in the difference in quality of care in LTC care homes, where LTC homes and their residents of for-profit ownership face poorer quality of care.
Staffing, Wages & Conditions of Care
There is no care without staff. Inadequate staffing levels are one of the many factors contributing to the high rate of COVID-19 and deaths of residents in for-profit LTC homes.
Low levels of staff have been an ongoing crisis prior to the pandemic. Unsafe staffing levels are related to the fact that staff that work in for-profit chains are paid less. For-profits also hire more casual and part-time staff to avoid providing staff benefits. At the same time, shareholders and investors receive tens of millions per month in profits. As cited in the Ontario Legislature in 2007, Karen Sullivan, the executive director of the for-profit LTC lobby group, stated that for-profit LTC homes earn profits in part from the low wages for staff and charging higher fees to residents who have private rooms.
Staff also work in multiple health care facilities to compensate for the low wages from working in LTC homes. Many staff quit because of the working conditions, low staffing levels, and unlivable wages of care. Two systemic reviews examined one Canadian study and found that staff working under for-profit ownerships had higher staff turnover compared to non-profit ownerships. Understaffing is also correlated with higher rates of injuries for staff. According to a study that examines staffing and worker injury in LTC homes, there is a proportionate relationship between staffing levels and the health and well-being of staff.
Ultimately, unsafe working environments and understaffing in for-profit LTC homes lead to the harm and deaths of residents. Care is not possible without staff, and the working conditions for staff in LTC homes are the conditions of care for the residents.
Living Conditions
More for-profit LTC homes that do not meet current design standards than non-profit and publicly owned LTC homes. These outdated buildings contributed to the higher rates of COVID-19 and deaths in for-profit LTC homes compared to non-profit LTC homes. Residents infected with COVID-19 were still being kept in the same room as healthy residents, increasing the risk for contagion. The lack of care and compassion for residents and the focus on profits from these for-profit operators is unethical and unacceptable.
In one example of a for-profit LTC home, Orchard Villa, there was a terrible outbreak with at least 70 residents who died as a result of COVID-19 alone, and others died of dehydration and malnutrition. The military, who were sent in to help, found terrible living conditions at the homes, including:
- Residents’ mattresses put on the floor to prevent them from standing or walking
- Mattresses without linens
- Uncleanliness
- Living with flies and cockroaches
- Living in the smell of like rotten food
- Overcrowding
- Poor infection control
A study that examined the admission experience of residents into for-profit LTC homes compared to non-profit LTC homes found a disproportionate relationship to the quality of living conditions and stress. For-profit facilities have fewer services and provide lower comfort and security, which increases residents’ stress levels.
What can you do?
- Learn more and stay updated on issues related to long-term care/chronic care: https://www.ontariohealthcoalition.ca/index.php/category/key-issues/long-term-care-chronic-care/
- Make this a key issue in the upcoming provincial election
- Contact your local MPP to raise concerns related to for-profit long-term care homes
- Find out who your local MPP is: https://www.ola.org/en/members/current
- Get involved with your local coalition
- Contact information for Ontario Health Coalition and your local coalition: https://www.ontariohealthcoalition.ca/index.php/contact-us/head-office/
- Share this briefing note widely to raise awareness
Click here for printable version


