REPORT: Crisis Unabated: The Failure to Improve Dangerously Low Care Levels in Ontario’s Long-Term Care Homes
Posted: May 18, 2022
(May 18, 2022)
Click here for printable version of report found below.
Summary of Findings
After enormous public pressure, the Ford government committed to improving care levels in Ontario’s long-term care homes. Even though residents were dying literally by the thousands in the pandemic, the plan which is very simple and could have been forged in a matter of a few weeks, took almost a year to be released, and then it delayed any improvements at all for more than another year. The plan has been repeatedly re-announced ever since.
The most important aspect of the plan – the first incremental improvement in care – was supposed to happen by March 31, 2022. At that point, the target was to have care levels increase by 15 minutes from 2.75 hours of care per resident per day to 3 hours of care per resident per day. This was the first step in a painfully slow plan to ratchet care levels up to 4 hours per resident per day by 2025. Many groups, including the Long-Term Care COVID-19 Commission and the Ontario Health Coalition have called for the government to move more quickly on this issue. However, despite repeated announcements of tens of thousands of new staff and improved care families and staff overwhelmingly contend that care has not improved.
Working with families, family councils, workers and their unions, from March – May 13, the Ontario Health Coalition sought actual staffing schedules from approximately 70 long-term care homes to see if Ontario has met that first promised target of 3 hours of care per resident per day. This report contains the results of that effort. A significant number of the homes refused to provide this information to their own families and family councils, despite the fact that the residents and their families are paying for their care. This is unacceptable. The homes are paid for by public funds and residents’ fees and must be made accountable to the public. In the United States this information is required reporting and is openly published.
In the end, we were able to get staffing data from approximately half of the homes. Some of it was unusable because the data we requested was not provided, was incomplete or was unintelligible. In the end, we have in depth actual staffing levels data from 23 homes. These facilities were not selected on any basis other than family councils, families or care workers were able to get the data from them.
The data we were able to get is disturbing. The evidence holds that a safe level of care for average acuity (and Ontario has very high acuity) would be at minimum 4-hours per resident per day. None of the homes are anywhere near that level. In the 23 homes where we were able to do an in-depth calculation of the actual staffing hours, the care levels range from a low of 2.25 hours of care per resident per day to a high of 3.34 hours. In context, the government’s expert staffing panel report found that the average level of care at the start of the pandemic was 2.75 hours of care per resident per day.
At 2.25 hours of care, a resident would not have their teeth brushed, they would not be bathed as they are supposed to be, staff would have little or no time to talk with them, they would not be toileted and would be left in wet incontinence pads, they would not have their skin breakdown properly assessed, or their pain, they would likely not be turned as required to prevent bedsores, they likely would not get enough water and juice and become dehydrated. Low levels of care mean that feeding is rushed and their lives are turned into a series of sporadic rushed tasks. Such a low level of care is dangerous, dehumanizing, and is proven to cause serious health crises and suffering.
Out of the 23 homes, nine – or more than a third — have care levels below 2.75 hours per resident per day. Seventeen of the 23 homes – or 74 percent – have care levels below 3 hours per resident per day. Only six of the homes have met the target of 3 hours of care per resident per day.
The homes cover regions from the Southwestern to eastern borders of Ontario, from as far Northwest as Thunder Bay to the Quebec border in the Northeast. See the chart below for detailed findings.
Obviously, this information is incomplete and just a start. However, we believe it fairly represents what we are hearing from families and residents across the province. It is critical that staffing levels be improved for real. It is equally crucial that regular open reporting of these care levels in every long-term care home be made available to residents, their families and the public.
Summary of the Issues & Promises
For decades, long-term care residents, families, unions and advocates have been working to win improved care levels in Ontario’s long-term care homes. Despite repeated media exposés revealing hair-raising negligence, sustained attention was almost impossible to garner. The lobby of the for-profit long-term care industry has been powerful since at least the 1990s, and progress towards unannounced comprehensive inspections, enforcement and fines has been achieved and then repeatedly rolled back. Harder still has been the struggle to win improved care levels. Care cannot happen without staff, and a deadly combination of austerity budgets and a powerful lobby for deregulation has, time and again, derailed efforts to win measures that would have increased funding for staff and made hard and fast requirements that public funding and residents fees to go to increasing care. Ontario’s public interest forces have, for more than a decade, coalesced around a key demand for a minimum care standard that would require all Ontario long-term care homes to provide a safe and dignified level of care. Yet care has not improved. In fact, in many long-term care homes it is the same or less than it was at the beginning of the pandemic, and it was in crisis then.
One cannot overstate the extent to which the pandemic has devastated long-term care. By May 2020, 1,377 seniors had died in just a few short months of COVID alone in the homes. The military had to be called in, and although they only went into six facilities, their harrowing accounts of the conditions of life and care catapulted long-term care into the international spotlight. However, even before the pandemic, we had been raising the alarm about the staffing crisis that had emerged as a result of poor working conditions in the sector. In 2019 we released a report Situation Critical about woefully inadequate levels of care and increasing violence in Ontario’s Long-Term Care. In December 2019, we released another report Caring in Crisis: Ontario’s Long-Term Care PSW Shortage commissioned by Unifor, based on round tables with more than 350 participants including home operators and administrators, PSWs, union representatives, family councils, seniors, college staff who develop/coordinate PSW courses, local health coalitions and other long-term care advocates we detailed the extent of the crisis. Unifor delivered the report to Premier Ford by hand.
The military reports released in late May 2020 made the situation impossible for political leaders to ignore. On May 27, Premier Ford vowed to “fix” long-term care. He said there would be accountability and justice, that the homes would be inspected, that residents would be protected, that all options were on the table, that homes would face penalties, that licenses would be revoked, and that criminal charges would be laid if warranted. He said “no stone will be left unturned”. Today, more than 4,500 residents have died in Ontario’s long-term care homes of COVID alone. That number does not include what we estimate to be thousands more who have died of neglect and a failure to provide care.
The government’s expert staffing panel, launched in February 2020 in response to our pressure regarding the staffing crisis, reported in July 2020. Instead of kickstarting action as we expected, the report was followed by another delay of six months. Instead of taking immediate action as the Quebec government did after the first wave, Ontario’s government promised to come up with a staffing plan by the end of the year. Little did we know then that the staffing plan would delay the first incremental improvement to care levels until April 2022.
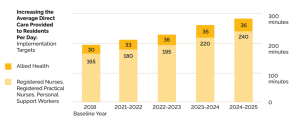
In December 2020, the government finally released their staffing plan. Under continued pressure to address the long-term care (LTC) staffing crisis, the Ministry of LTC set a target timeline to achieve 4 hours of care (RN, RPN, PSW, worked hours) by 2025. As pictured below, using 2018 as the baseline, the Ministry claims there was an average of 165 minutes (2 hours and 45 minutes) of care per resident per day. Their timeline proposal committed to an increase in care to 180 minutes, or 3 hours of care per resident per day, by March 31, 2022.
Our goal in writing this report was to measure actual levels of care in an array of LTC homes and see how they compare to that target of 3 hours of hands-on care per resident per day that was supposed to be reached by March 31. This report contains our findings. It is a moral imperative that whichever political party forms the next government in Ontario, the neglect of the elderly and chronic care residents in long-term care stop. The scale of the horrors that have happened in the pandemic, and before, require a real “never again”.
Graph 1. Target increase in care levels per resident per day from the Ministry of Long-Term Care Ontario’s Long-Term Care Staffing Plan 2021-2025
Please note: the daily hands-on care for residents shows in the bottom section of each bar in the graph. It shows the target for daily hands-on care provided by RNs, RPNs, PSWs (and should exclude the Director(s) of Care who are management staff, and any aides who are not actual PSWs).
Results:
| Ownership Type | Location | Hours of Care Per Resident Per Day | |
| Home 1 | For-Profit | Sault Ste. Marie/Algoma | 2.49 |
| Home 2 | Municipal | Eastern Ontario | 3.06 |
| Home 3 | Non-Profit but managed by for-profit | Sault Ste. Marie/Algoma | 2.7 |
| Home 4 | Non-Profit but managed by for-profit | Thunder Bay/Superior North | 2.57 |
| Home 5 | Municipal | Thunder Bay/Superior North | 3.06 |
| Home 6 | Non-Profit | Sault Ste. Marie/Algoma | 2.82 |
| Home 7 | For-Profit | North Huron/Huron County | 3.11 |
| Home 8 | Non-Profit | Elgin County/SW Ontario | 3.17 |
| Home 9 | For-Profit | Niagara | 2.39 |
| Home 10 | Non-Profit | Eastern Ontario | 2.25 |
| Home 11 | For-Profit | Eastern Ontario | 2.8 |
| Home 12 | Non-Profit | Toronto | 2.85 |
| Home 13 | For-Profit | London | 3.07 |
| Home 14 | Non-Profit but managed by for-profit | Toronto | 2.97* |
| Home 15 | Non-Profit | GTA | 3.34 |
| Home 16 | Non-Profit | Mississauga | 2.85 |
| Home 17 | For-Profit | Sarnia/Lambton | 2.87 |
| Home 18 | For-Profit | Sault Ste. Marie/Algoma | 2.36 |
| Home 19 | For-Profit | Southwestern Ontario | 2.47 |
| Home 20 | Non-Profit | Durham/GTA | 2.9 |
| Home 21 | For-Profit | Toronto | 2.82 |
| Home 22 | For-Profit | NE Ontario | 2.61 |
| Home 23 | Non-Profit | Toronto | 2.7 |
Average hours of care
| Average hours of care per for-profit home | 2.69 |
| Average hours of care per non-profit home | 2.86 |
| Average hours of care per municipal home | 3.06 |
* This data was reported by the home’s administrator from payroll and it likely overstates the hours of care by including hours that are paid hours but not worked hours.
- 9 of 23 homes have care levels below 2.75 which was what the government reported care levels to be at the beginning of the pandemic. This represents almost 40 percent of the homes.
- 17 of 23 homes have care levels below 3 hours which was the target that was supposed to be achieved by March 31, 2022. This represents almost 75 percent of the homes.
- Only 6 homes have care levels above 3 hours.
Appendix.
This is the method by which we collected the data.
| Please send this form in to the Ontario Health Coalition at ohc@sympatico.ca with ATTN: NATALIE STAFFING SURVEY in the subject line.
Your Name: Your email: Your phone number: Name of the long-term care home: City/town the long-term care home is located in: Is the home public (municipal), non-profit, or for-profit: How many residents on the unit?: |
|||||||
| Please use this part only if it is helpful. You can also send in the staffing schedule, with the actual staff present, noted as accurately as possible. Note: We do not need staff names. | |||||||
| Day 1 Date: | Day 2 Date: | Day 3 Date: | Day 4 Date: | Day 5 Date: | Day 6 Date: | Day 7 Date: | |
| MORNING shift
PSWs: How many? Please note each of their start times/End times |
|||||||
| RPNs: How many? Are any of the RPNs split between multiple units? If so, please note how many units each is covering.
Please note each of their start times/End times |
|||||||
| RNs: How many? Is this RN for more than one unit? If so, please describe how many units they cover if possible.
Start time/end time |
|||||||
| AFTERNOON shift
PSWs: How many? Please note each of their start times/End times |
|||||||
| RPNs: How many? Are any of the RPNs split between multiple units? If so, please note how many units each is covering.
Please note each of their start times/End times |
|||||||
| RNs: How many? Is this RN for more than one unit? If so, please describe how many units they cover if possible.
Start time/end time |
|||||||
| EVENING-NIGHT shift
PSWs: How many? Please note each of their start times/End times |
|||||||
| RPNs: How many? Are any of the RPNs split between multiple units? If so, please note how many units each is covering.
Please note each of their start times/End times |
|||||||
| RNs: How many? Is this RN for more than one unit? If so, please describe how many units they cover if possible.
Start time/end time |
|||||||
| Any extra staff: please include details | |||||||