REPORT: Long-Term Care Survey Report Released by Kawartha Lakes Health Coalition, Northumberland Health Coalition, and the Peterborough Health Coalition
Posted: June 22, 2021
(June 22, 2021)
Introduction
We are here to discuss the problems in Long Term care because of an anonymous survey completed by front-line workers within Long-Term Care workplaces in Kawartha Lakes-Peterborough-Northumberland regions. Long-Term Care Homes is the term now used for nursing homes, charitable homes, and municipal homes for the aged. We are not talking about Retirement Homes which are not regulated and are not supposed to be health care facilities.
Chronic underfunding and privatization of health care has had an increasingly negative impact in Long-Term care.
Decades of underfunding, understaffing, part-time work, no sick pay, and a focus on profits over care have deeply eroded Ontario’s Long-Term Care system.
We even have members of our group who were participants in the DIGNITY and Justice campaign back in 1996. This was when Conservative Premier Mike Harris repealed the standards of care legislation for Long-Term care.
During COVID-19, the system reached its breaking point and almost 4,000 people died in LTC.
As we continue to make our way through the pandemic, we wanted to get an update from LTC frontline staff locally and regionally to find out about their experiences and to see if they matched what we were being told provincially
The stories did match, so we will be providing you with the survey details, a brief analysis, and our recommendations for action.
Survey questions and responses:
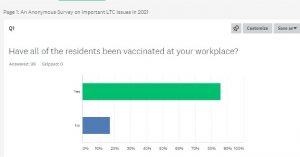
Q1: Have all of the residents been vaccinated at your workplace?
Yes – 85.86%
No-17.17%
Q2: If all residents at your workplace have not yet been vaccinated, what is the planned date of completion?
- 2021
- Majority of the residents are vaccinated. However, the ones who are not, it is because the families did not consent for the resident to receive it.
- Not sure
- Some residents chose not to be vaccinated
- Based on age and vaccine availability.
Q3- Have all of the unionized staff been vaccinated?
Yes – 23.23%
No – 78.79%
Q4: If all unionized staff at your workplace have not yet been vaccinated, what is the planned date of completion?
- September 2021
- Not sure if all the unionized staff are vaccinated yet. Those who are not, either have not decided to yet or only received 1 dose so far.
- Those that want it have received it and if the ones that don’t have it want it, they still have the opportunity to get it. No time lines
- Varies and some don’t want it and we don’t know who has or hasn’t had even 1st dose
- I am weighing my options of which vaccine to get as a 27-year-old on birth control who smokes and is high risk for blood clots
- As soon as vaccines become available. Some members chose not to be vaccinated
- July
- June 2021 when more vaccines available
- People have the right to do as they wish with their body
- Don’t know
- Ran out of vaccine. I’m still waiting
- I believe we received emails mid may regarding our second vaccine so we can be fully vaccinated
- Not sure, second dose date was canceled and unsure when it will be rescheduled
- Those who want it, have been vaccinated
- No known date of completion
- All have their first vaccination (which they began getting at the end of February), however the second dose date has been pushed out.
- Waiting on 2nd dose appointment
- Would like the answer myself
- Nobody on medical leave or maternity was contacted by the employer and they have no plan to contact these people. they have specified its up to the staff to get their own
- Second vaccine hopefully in July 2021
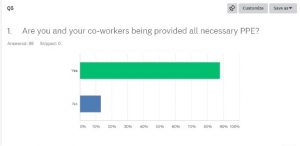
Q5: Are you and your co-workers being provided all necessary PPE?
Yes – 87.88%
No – 13.3%
Q6: If all PPE is not being provided, please list what is missing
- N95 with some groups where it is required.
- All is there and they have tons back up supply in basement due to shortages from last year. We are now prepared for years.
- Surgical masks do absolutely nothing to protect the staff. If Covid was as serious as they say it would be mandatory and we would all have N95
- We don’t have N95 masks
- Not all staff have had mask fit
- Are we supposed to be wearing N95 masks- cause all we are wearing are surgical?
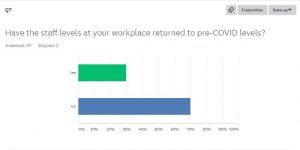
Q7- Have the staff levels at your workplace returned to pre-COVID-19 levels?
Yes- 29.90%
No- 70.10%
Q8: How often do you find yourself working short?
- Daily- 76%
- 50 % of the time – 12%
- Didn’t answer – 7%
- Not in my role/Not applicable =2%
- Once or twice every few weeks – =.09%
Q9: What do you feel is the biggest issue that needs to be resolved at your workplace in order to provide full service delivery to the residents at your workplace?
- Increased staffing – 70%
- Better management – 29%
- More money – 21%
- More Full-time – 8%
- Better/more vacation – 3%
- Improved COVID health and safety measures – 2%
- Better Union – .09%
- Childcare – .09%
- Every LTC home should have a BSO Team – .09%
- Better equipment – .09%
- Childcare- .09%
- Lack of Linen – .09%
- Nothing-.09%
Q10: In which community is your workplace located?
- Kawartha lakes – 43%
- Peterborough – 41%
- Northumberland- 15%
- Out of the area – 1%
Analysis
There are many of us, (family members, staff, and community activists) in and outside of LTC facilities that have been fighting for improvements to LTC facilities. since standards of care were removed by the conservative Mike Harris government in the mid-90s. We have continued that fight ever since because no-one in government since the mid-90s has had the political will or compassion to fix the real problems in LTC.
As one example in this continuing battle for improvements (In 2019, pre COVID-19), at a Northumberland press conference, it was reported that there were nearly 80,000 residents in Ontario’s Long-Term care homes with more than 33,000 Ontarians waiting for space. Wait lists were larger than an entire small town, larger than Lindsay and Port Hope combined, for example. In fact, at that time, Ontario ranked second last in Canada in the number of Long-Termcare beds per capita.
It was reported at that time (pre-COVID) that actual levels of care were a major problem too. In fact, pre-COVID, it was reported by LTC staff that:
Levels of care was too low to meet basic safety requirements and research showed that they have been declining
Acuity (heaviness and complexity) of residents had soared as successive Ontario governments had cut hospital beds to the lowest rates per capita amongst all provinces in Canada. Almost no other country and no other province had cut hospital beds to such an extreme as Ontario.
As a result, heavier care patients were offloaded from hospitals into Long-Term care. But care levels in LTC are not the same as in hospitals. Yet, it was found that fully one half of Ontario’s chronic care hospital beds had been closed and the acuity of residents in Long-Term care matches chronic care hospital level. BUT the funding of Long-Term care only matched 1/3 of the hospital rate.
The Bottom Line?
Patients had been moved out to reduce cost at the expense of their health and safety. Oh yes, there was no question, Long-Term care homes pre-COVID-19 were already the chronic care and psychogeriatric care hospitals of yesteryear but without the resources.
For families who could afford it, they spent many thousands of dollars hiring-in extra care. For those who couldn’t afford it, they suffer with inadequate care.
Considering the above, to hear that staffing levels has not even returned to pre-COVID-19 levels is very concerning!
Residents, front-line workers, families, friends, relatives and concerned Canadians have and continue to speak out but the Ontario government has been in denial and is not listening to anyone about the need to act now to address the low levels of staff and care.
Ten per cent of all COVID-19 cases and 69 per cent of COVID-19 deaths occurred in Long-Term care homes, according to the latest data tracker from the National Institute on Ageing at Ryerson University.
Across Canada, 28 percent of Long-Term care facilities are for-profit, the Canadian Institute for Health Information (CIHI) says. In Ontario, they account for 57 percent. These for-profit homes had “outbreaks with nearly twice as many residents infected” and 78 per cent more resident deaths compared with not-for-profit homes, the Ontario COVID-19 Science Advisory Table showed.
Ontario currently has no legislated minimum staff to resident ratio requirement for Long-Term care facilities. With current levels of acuity in Long-Term care and based on the best of value available evidence, a regulated minimum average of 4 hours of daily hands-on direct care staffing is required to prevent harm and improve outcomes. Today, there are often more tasks to complete than there is staff available. To get the job done means residents are fed too quickly, cannot get enough food down, resulting in residents risking dehydration etc. It means little time for bathing or repositioning to prevent sores and contractures. It means no friendly visits or socialization for lonely or depressed residents. As a frontline worker reported at a previous press conference – even without getting all the work done, Healthcare workers are still going home after their shifts sore and hurt themselves from the physical energy they exert every day.
The COVID-19 crisis has drawn attention to the inconsistent regulations, low standards of care, and poor working conditions in Ontario Long-Term care facilities, in some provinces more so than others.
The ongoing systemic weaknesses in Ontario Long-term care facilities made ever so much worse by COVID-19 increased the numbers and severity of COVID-19 cases to which Long-Term care residents and staff were exposed.
In British Columbia, a more modern infrastructure with fewer multi-units, with government initiated staffing controls, with pay increases and the provision of personal protective equipment (PPE) kept Long-Term care infections relatively low. In contrast Ontario did not take the same approach to stopping the rate of transmission of the virus as early in the Pandemic as BC. This meant the Ontario approach was less efficient and likely more costly, relying on full scale investigations and the deployment of the military.
By failing to quickly invest in protective equipment and staffing capacity, Ontario struggled to contain outbreaks and saw death rates that were 14 – 23 times higher respectively (in May 2020) compared with British Columbia.
Ontario was also not like Quebec. In June 2020, Quebec went out to recruit the thousands of staff needed and fast tracked intensive, paid training, improved wages and working conditions to retain staff, accessed military support for the Long-Term care homes in crisis where local hospital teams were not available to come in. Quebec did that well before Ontario did.
In addition, in Ontario, chronic underfunding driven by a focus on cost containment and profit due to steep growth in healthcare costs associated with an aging population has made a bad situation that much worse. Since the start of the pandemic, almost 4,000 Long-Term care residents have died because of COVID-19.
In the first wave of the pandemic, Long-Term care facilities saw 80 per cent of Canada’s total COVID-19 deaths. Outside of Quebec and Nova Scotia, deaths in Long-Term care increased in the second wave.
Inspections could also be important mechanisms for ensuring that LTC homes are prepared to prevent and manage infectious diseases. Ontario required annual inspections of all LTC homes by the Ministry of Long-Term Care. Before 2018, almost all LTC homes in Ontario received comprehensive inspections. However, in late 2018, Ontario transitioned to a risk-based framework where narrower inspections are conducted in response to critical incidents and complaints. As a result, although there were about 2800 inspections in 2019, most were related to complaints or critical incidents, and only 9 of 626 (1.4%) LTC homes in Ontario received a comprehensive inspection.
What happened during the COVID-19 pandemic DID NOT happen in a vacuum.
Yet knowing and hearing all this evidence- somehow, we are expected to wait another 4 years? For whom? No-one knows which party will be the government in another four years.
“The COVID-19 pandemic has made the holes in our social safety net and the failures in our social infrastructure painfully obvious. A horrific example of these failures is the impact of the pandemic in Long-Term care (LTC) homes.
Even CCPA reports that a fairly paid workforce with adequate staffing levels is a crucial first step toward a quality Long-Term care system in Ontario.”
“Ontario’s beleaguered Long-Term care system needs a funding injection of $1.8 billion a year to bring wages and staffing up to recommended levels of quality of care and safety, according to a new study from the Canadian Centre for Policy Alternatives (CCPA).
“The most potent factor shaping quality of care and safety of both residents and workers in Long-Term care facilities is staffing levels,” said Sheila Block, CCPA Ontario senior economist and co-author of What Does it Cost to Care? “The ongoing tragedy in Long-Term care during COVID-19 is the sad result of successive provincial governments’ relentless underfunding of the sector.”
Bringing hands-on care levels up to 4.1 hours per resident per day—a widely recognized standard for quality care—would require a 51 per cent increase in caregiving hours and cost an additional $1.6 billion in 2020-21, the CCPA study estimates. Block and co-author Simran Dhunna estimated it would cost a further $285 million a year to bring up wages for non-union registered nurses (RNs), registered practical nurses (RPNs), and personal support workers (PSWs) to average union rates.”
Without appropriate staffing numbers that includes highly developed retention policies, (wages, benefits, full-time hours), levels of care will remain too low to meet basic safety requirements. The facts are that it has already been demonstrated by organizations such as the Ontario Health Coalition that Acuity levels (heaviness and complexity) of residents has soared as Ontario governments have cut hospital beds to the lowest rates amongst Canadian provinces.
As a result of those cuts, heavier and complex care patients are offloaded from hospitals into Long-Term care facilities. But care levels are not the same. For example, the Ontario Health Coalition found that fully 1/2 of Ontario’s chronic care hospital beds have been closed and the acuity of residents now in Long-Term care matches the chronic care hospital level. But the funding of Long-Term Care is 1/3 of that rate. Clearly patients have been moved out to reduce costs at the expense of their health and safety.
AS Dr. Samir Sinha, Director of Geriatrics at Mount Sinai Hospital in Toronto, said on CTV’s Your Morning, “More staffing tends to mean better care.”
Conclusions and recommendations:
According to the science table of Ontario, the Province of Ontario has 626 licensed LTC homes and 77,257 long-stay beds; 58% of homes are privately owned, 24% are non-profit/charitable, 16% are municipal. LTC homes were strongly affected during Ontario’s first and second waves of the COVID-19 pandemic.
In Haliburton and Kawartha with a population of 93, 485 has 11 Long-Term Care Homes with 892 beds; Peterborough City and County with a population of 138,236 has 8 LTC homes with 1,111 beds; Northumberland County with a population of 73,754 has 8 LTC homes with 667 beds. (As reported pre- COVID-19 in 2019 by Central East LHIN). These numbers are placed here to provide readers with a better sense of the significance of the issue of LTC facilities and standards of care.
Now is the time to fix Long-Term care, not years from now.
We agree with the Hamilton Burlington and Oakville chapter of the Congress of Union retirees of Canada when they said that when Ford promised an iron ring around the Long-Term care homes – instead, the Ford government built a legislative Iron Wall of protection around the government and the owners and operators of private for profit Long-Term Care homes.
We are making every effort to bring and hold the public’s attention to an extremely important issue that has been exacerbated by a pandemic that has changed everything. This issue has been around for a long time and much has been promised but not delivered – time is against us.
Chronic underfunding and privatization of health care have had an increasingly negative impact, particularly in Long-Term Care, as has been made painfully obvious during COVID. Decades of underfunding, understaffing, poor working conditions, high levels of violence and a focus on profits over quality care have eroded Canada’s system of Long-Term Care to the breaking point, leaving us tragically unprepared to protect the lives of our most vulnerable. Four out of five COVID-related deaths in Canada have been either residents or staff of Long-Term Care homes – the highest proportion in the world.
Those in power have ignored strong criticisms of the living and labour conditions in Canada’s LTC system for decades. But the research is unambiguous: for-profit facilities offer comparatively substandard care. In fact, the CMA recommended a transition away from private facilities as far back as 1984. It should come as no surprise that LTC homes were woefully unprepared to survive the impact of the virus.
Therefore, we call upon the province to implement the following measures:
- End for-profit Long-Term Care homes.
- Follow through on your promise to hire additional qualified staff without fast-tracking undertrained students or reducing qualifications.
- Ensure all LTC residents receive at least the minimum four hours of direct hands-on care per day your government promised.
- Set a minimum pay standard, consistent with the hospital sector, for frontline LTC staff that includes not only personal support workers and other medical professionals, but also cleaning, food service and administrative staff.
- Ensure a minimum of 70 per cent of staff at each LTC home are full-time.
We also strongly advocate for Paid Sick Time and access to Benefits for LTC staff, enabling them to make a decent living and eliminating the need to work more than one job in multiple locations. This is good for residents as well as workers. Stability for the people providing the care is key to ensuring a healthy and robust system of caring for our most vulnerable.
IN LTC, frontline workers working conditions are LTC residents’ living conditions.
We have and will continue our plan to lobby hard for these and other reforms promised by Doug Ford way back at the beginning of this pandemic. People have been needlessly dying out there and it will happen again — it is not a question of if but when. We need to fix this NOW.
Resources
We have listed these Resources for three reasons
- Evidence to help back up our statements made earlier in this short brief
- As educational assistance on the issues
- Evidence of how very many organizations are lobbying the government for change and improvements in LTC. There are of course more organizations that have not been included here.
The list is not made in order of any priority
Ryerson University Long Term Care COVID-19 Tracker
https://ltc-covid19-tracker.ca/
Why The Problem of Privatization in Long-Term Care Goes Beyond Corporate Ownership: Low-quality, high-cost long-term care is a symptom of policies aimed at cutting public services and cutting taxes.
Graphs and tables of COVID-19 data for Ontario residents and staff living or working in Ontario’s long-term care homes
https://covid-19.ontario.ca/data/long-term-care-homes
Situation Critical: Planning, Access, Levels of Care and Violence in Ontario’s Long-Term Care
“A fairly paid workforce with adequate staffing levels is a crucial first step toward a quality long-term care system in Ontario.”
What does it Cost to Care?
The COVID-19 pandemic has made the holes in our social safety net and the failures in our social infrastructure painfully obvious. A horrific example of these failures is the impact of the pandemic in long-term care (LTC) homes. This paper provides a cost estimate for adequately funded caregiving in Ontario long-term care homes, showing that it would cost about $1.8 billion to increase care levels and equalize wage rates across the sector in this fiscal year. This equates to just over 1% of overall provincial program spending in Ontario.
Ontario nursing homes badly prepared for COVID-19 pandemic, auditor general says (includes auditor- general’s report):
Ontario Long-Term Care COVID-19 Crisis: 100 Organizations Sent Clear Message to Premier Ford, “This is an Emergency, We Need Action Now”
Examples of LTC Outbreak Media Reports in Kawartha Lakes:
COVID-19 outbreak at Kawartha Lakes long-term care home leads to deaths, staffing issues- 34 of the 66 staff members have reported feeling ill, Ontario facility asks for more staff
COVID-19: Outbreak at Lindsay long-term care ‘reflection’ of single-day record 35 new cases in Kawarthas
Examples of LTC Outbreak Media Reports in Peterborough
COVID-19 outbreak confirmed at Fairhaven Long Term Care in Peterborough
Fairhaven outbreak declared May 21, 2021
Examples of LTC Outbreak Media Reports in Northumberland
Hope Street Terrace Long-Term Care in Port Hope Dealing with COVID-19 Outbreak With No Vaccine In Sight
Another COVID-19 death in Northumberland County
Doctor says Canada underfunding long-term care amid call to end for-profit homes
ONTARIO: Advocates call for national long-term care standards
In the first wave of the pandemic, long-term care facilities saw 80 per cent of Canada’s total COVID-19 deaths. Outside of Quebec and Nova Scotia, deaths in long-term care actually increased in the second wave.
https://www.cbc.ca/news/politics/long-term-care-pandemic-covid-1.6036397
Ontario Long term care Commission Interim Report
http://www.ltccommission-commissionsld.ca/ir/
Ontario Long Term Care Commission Final Report
http://www.ltccommission-commissionsld.ca/report/index.html
Science Table- COVID-19 Advisory for Ontario COVID-19 and Ontario’s Long-Term Care Homes
https://covid19-sciencetable.ca/sciencebrief/covid-19-and-ontarios-long-term-care-homes-2/
Video presentation
https://www.youtube.com/watch?v=xLAi3c-PqXg&ab_channel=OntarioCOVID-19ScienceAdvisoryTable
Ontario Science Table Brief on COVID-19 and LTC homes (Text)
https://covid19-sciencetable.ca/sciencebrief/covid-19-and-ontarios-long-term-care-homes-2/
CARP- We have a crisis in long-term care in Canada.
Now and moving forward, we need a commitment from governments to eradicate the systemic vulnerabilities exposed by COVID-19 which threaten residents in long-term care. Since the coronavirus hit long-term care homes, CARP has been actively calling on government to prioritize care for seniors.
https://www.carp.ca/2020/04/15/covid19-longtermcare/
Military Report on Ontario Long Term Care
https://assets.documentcloud.org/documents/6928480/OP-LASER-JTFC-Observations-in-LTCF-in-On.pdf
The Crisis of Privatized Care in Ontario
https://healthydebate.ca/2020/12/topic/crisis-privatized-care-in-ontario/
COVID-19 in long-term care homes in Ontario and British Columbia
https://www.cmaj.ca/content/192/47/E1540
Restoring trust: COVID-19 and the Future of Long term care
Ontario Auditor General Report on Long term care
https://www.auditor.on.ca/en/content/news/specials_newsreleases/newsrelease_COVID-19_en202104.pdf
Click here for printable version of report